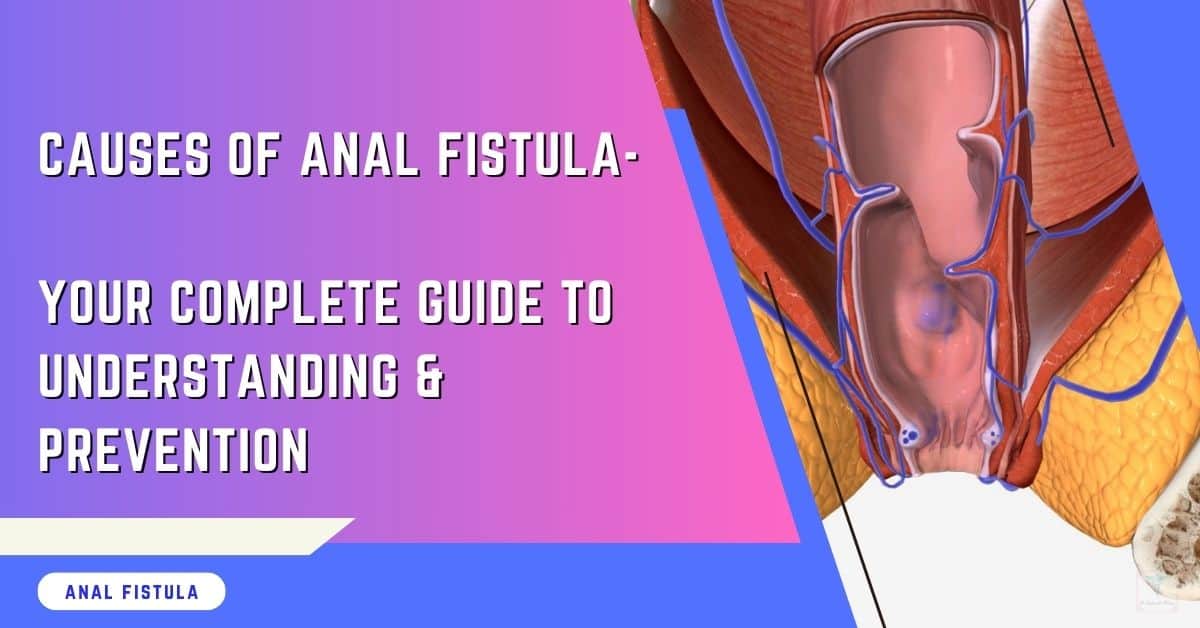
Navigating the complexities of health issues can be daunting, especially when it comes to recognizing the symptoms of anal fistula. This condition, though not widely discussed, affects many, and understanding its signs is crucial for timely intervention.
I’ve previously shared the causes of Anal Fistula. And in this guide, you’ll uncover the key indicators to watch out for, from discomfort and irritation in the anal area to more pronounced symptoms such as abnormal discharge.
Armed with this knowledge, you and your loved ones can take proactive steps toward diagnosis and treatment, ensuring better health outcomes and peace of mind.
Symptoms Of Anal Fistula: Quick Facts
- Stay Alert to Symptoms: Recognize early signs of anal fistulas, such as discomfort, swelling, and abnormal discharge near the anus, to seek timely medical intervention.
- Seek Professional Help: Don’t hesitate to consult a healthcare provider if you suspect an anal fistula, as early diagnosis can lead to more effective treatment.
- Understand the Causes: Knowing that conditions like Crohn’s disease or previous surgeries can lead to fistulas helps in understanding your risks and managing your health proactively.
- Learn About Treatment Options: Be informed about the various treatment methods available, including surgery, which is often necessary to heal a fistula.
- Be Aware of Surgery Risks: Understand potential complications from surgery, such as infection or incontinence, to make an informed decision about your treatment plan.
- Follow Through with Recovery: Adhere to post-surgery care instructions and lifestyle adjustments to prevent recurrence and ensure a smooth recovery process.
Recognizing Symptoms Of Anal Fistula
- Persistent PainIf you’re experiencing constant and throbbing pain near your anus, it could be a sign of an anal fistula. This discomfort often gets worse when you sit or move around. During bowel movements or even when coughing, the pain might intensify. It’s crucial to seek medical evaluation if this type of pain persists, as it’s not something that will go away on its own.
- Unusual DischargeAnother telltale symptom is the presence of smelly discharge from the area around the anus. You might also notice pus or blood passing during bowel movements. This is not only uncomfortable but also a sign that something abnormal is happening in your body. Seeking medical advice for any unusual discharge is essential to get to the bottom of the issue ( no pun intended!).
- Skin IrritationSkin irritation around the anus can be both uncomfortable and embarrassing. This irritation often stems from discharge and moisture in the area, leading to discomfort and potential skin damage. Implementing a gentle skincare routine can help alleviate some of this irritation, but it’s also important to address the underlying cause.
- Recurrent InfectionsThe risk of recurrent infections is high with an anal fistula. These infections may present with swelling, redness, and fever, signaling that your body is fighting off invaders. Prompt treatment is vital to prevent further complications and discomfort.
When To Seek Medical Advice For Anal Fistula?
- Persistent SymptomsIf you notice symptoms like discharge and pain, know they may persist without treatment. Over time, these symptoms can worsen. It’s crucial not to ignore them. Seeking medical help is a step towards relief and recovery.
- Severe PainSevere pain differs from persistent pain in its intensity. It can significantly hinder daily activities. If severe pain comes with fever, it’s time for immediate medical attention. These signs might point to an emergency requiring urgent care.
What to Expect When Preparing For A Visit?
During your first visit, expect questions about your symptoms and medical history. Your healthcare provider will want details to understand your condition better. They may perform physical examinations and tests to diagnose an anal fistula accurately.
Before seeing your doctor or specialist, make a list of your symptoms. Include when they started and their severity. Note down any questions for your health care provider as well. Also, bring a list of all medications you’re currently taking.
Understanding Causes
Infection
Anal fistulas often stem from an abscess or infection near the anus. It’s crucial to pinpoint the source of this infection for effective treatment.
Conditions like Crohn’s disease heighten the risk of developing fistulas. They can make the situation more complex. Understanding this link helps in tackling the root cause, not just symptoms.
Chronic Conditions
Inflammatory bowel disease and other chronic conditions frequently contribute to anal fistulas. Managing these underlying issues is key to preventing fistula formation.
If you have a chronic condition, stay alert for new or worsening symptoms. This vigilance can lead to early detection and treatment, reducing complications.
Lifestyle Factors
Certain lifestyle choices might worsen your symptoms. Poor diet and hygiene practices are common culprits. To mitigate symptom severity and fend off recurrence, consider making some lifestyle changes, such as improving your diet and enhancing your anal hygiene.
Maintaining good anal hygiene is paramount. It helps not only manage current symptoms but also prevent future issues.
Differentiating Fistulas: Simple vs Complex
Symptom Severity
Assessing the severity of your symptoms is crucial. Severe pain, discharge, or bleeding indicates a more serious condition. These symptoms might mean your fistula tunnel is complex.
Treatment options vary based on symptom severity. Mild symptoms may need less invasive treatments. Severe cases often require surgery.
Keeping a symptom diary helps you and your doctor track changes. This record is vital for deciding on the best treatment plan.
Treatment Options
Several treatment options exist, from medication to surgery. The choice largely depends on the severity of your symptoms and your overall health.
Non-surgical therapies, such as antibiotics or special creams, might be enough for early-stage fistulas. However, most fistulas will always need some form of surgery. Complex fistulas often need surgical intervention in multiple stages.
Personalized treatment plans are essential. They should consider both the fistula’s characteristics and your health status.
Identifying Types Of Anal Fistula
Different types of anal fistulas affect your treatment plan and success rate. Knowing whether your fistula is simple or complex is key.
Simple fistulas have a direct tunnel and fewer complications. They’re easier to treat. Complex fistulas might involve multiple tunnels or affect more sensitive areas.
Accurate diagnosis ensures effective treatment. It prevents unnecessary procedures and promotes faster healing.
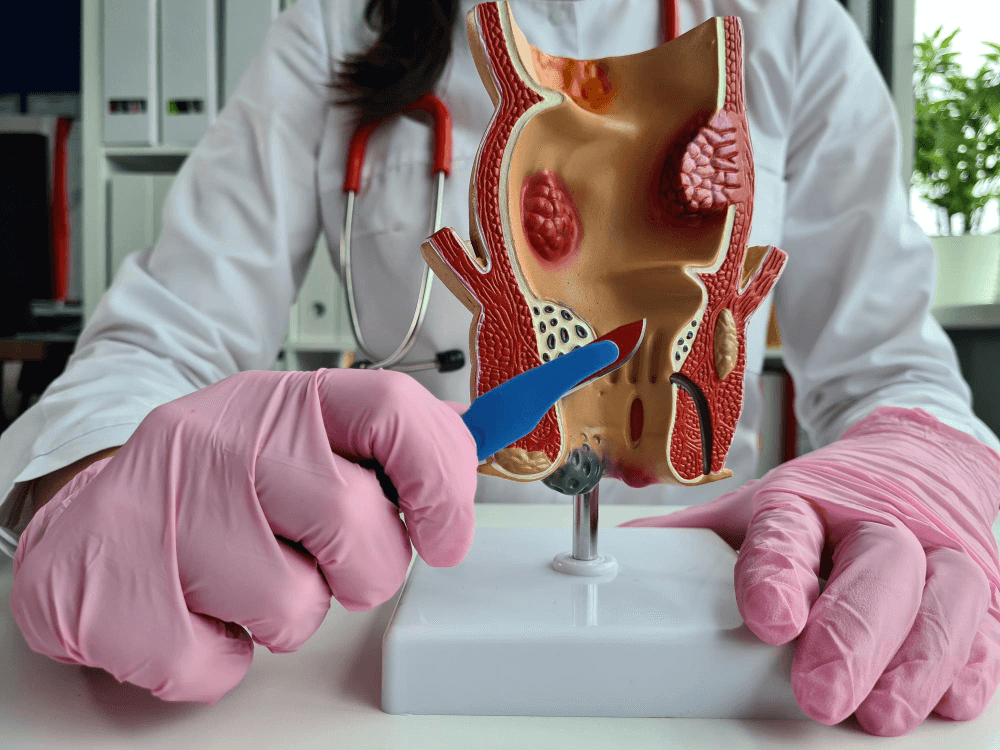
Treatment Overview

Surgical Options
Surgical procedures are often necessary to treat anal fistulas. The most common methods include fistulotomy and seton placement. Fistulotomy involves cutting open the entire length of the fistula so it can heal from the inside out. Seton placement uses a Silicone Tube to keep the fistula tract open for drainage over time.
Each surgical option carries its own risks and benefits. A fistulotomy is effective but might not be suitable for complex or high fistulas due to the risk of incontinence.
Seton placement is less likely to cause incontinence but may require multiple surgeries for complete healing. Multiple surgeries might be needed for complex fistulas, emphasizing the importance of discussing all possibilities with your provider.
Non-Surgical Therapies
Sometimes, non-surgical options like antibiotics or fistula plugs can manage symptoms. Antibiotics can treat infections associated with anal fistulas, while fistula plugs aim to block and eventually heal the fistula tract.
Non-surgical treatments are typically recommended when surgery poses too high a risk or if the condition is mild. However, their effectiveness varies, and following through with prescribed therapies is crucial for success.
Aftercare Essentials
Proper aftercare is vital in preventing a recurrence of an anal fistula. This includes diligent wound care, maintaining hygiene, and attending follow-up appointments with your healthcare provider.
These appointments are critical in monitoring your healing progress and ensuring that the treatment has been successful.
Surgery Risks
Common Complications
After exploring treatment options, it’s crucial to understand the risks associated with surgery for anal fistulas. Common complications include infection and recurrence.
These can significantly impact your recovery and overall health. An infection might require additional treatment, prolonging your recovery time. Recurrence of an anal fistula could mean undergoing more surgeries in the future.
It is essential to address signs of complications promptly. Symptoms such as increased pain, fever, or unusual discharge from the surgical site should not be ignored. They might indicate an infection or other issues that need immediate attention.
Managing Risks
Adhering to your treatment plan and follow-up care is vital to managing risks effectively. Your healthcare provider will guide you through the recovery process, but following their advice closely reduces the risk of complications.
Lifestyle modifications play a key role in preventing recurrence. These may include dietary changes to avoid constipation, maintaining good hygiene around the anal area, and avoiding activities that put excessive pressure on the pelvic floor.
Recovery Process

Post-Surgery Care
After surgery, it’s crucial to care for the bottom section to promote healing. You should gently clean the area after each bowel movement. Use mild soap and water. Avoid rubbing or scrubbing, which can irritate the site.
You might face restrictions on sitting or moving too much. It helps prevent pressure on the healing area. Follow your doctor’s advice closely.
Attending all post-operative appointments is vital. These visits allow your doctor to monitor your recovery and catch any issues early.
Activity Limitations
Activities that strain the bottom section, like heavy lifting, should be limited. Such actions can aggravate symptoms and delay healing.
To safely resume activities, start slow. Increase gradually as you feel comfortable. If an activity causes pain or discomfort, stop immediately.
Consider alternatives for risky activities. For example, swimming instead of cycling can reduce pressure on the sensitive area.
Follow-up Visits
Scheduled follow-up visits are crucial for a successful recovery. They might help prevent the recurrence of anal fistula.
During these visits, tests or examinations are expected to check the healing process. Be prepared to discuss any new or persisting symptoms with your doctor.
Preventing Fistulas
Lifestyle Changes
Making lifestyle changes can greatly reduce your risk of developing an anal fistula. Since fistulas often originate from issues in the digestive tract, adjusting your diet is crucial. Incorporate high-fiber foods to ensure smooth bowel movements. This reduces strain on the sphincter muscles and prevents complications.
Regular exercise and maintaining a healthy weight are also vital. They improve overall digestive health and minimize pressure on the anal opening and large intestine.
Good hygiene practices play a significant role in preventing infections that could lead to fistulas. After recovering from an anal fistula, keeping the area clean is essential. Use gentle cleaning methods and avoid harsh chemicals or soaps.
Regular Check-ups
After the recovery process, don’t underestimate the importance of regular check-ups. These appointments allow your healthcare provider to monitor your healing and catch any signs of potential issues early.
Ongoing monitoring is key to ensuring long-term health and preventing recurrence. Even if you feel fine, these check-ups can provide peace of mind and keep future problems at bay.
It’s crucial to maintain open communication with your healthcare providers. Share any concerns or symptoms you experience, no matter how minor they may seem. This proactive approach ensures you receive timely advice and intervention if needed.
Final Note From Dr. Rajarshi Mitra
Understanding the symptoms, causes, and treatment options for anal fistulas is crucial for managing this condition effectively. You’ve learned to recognize the signs, differentiate between types of fistulas, and understand the available medical interventions.
It’s essential to seek prompt medical advice if you suspect you have an anal fistula to prevent complications. The recovery process and surgery risks highlight the importance of closely following your healthcare provider’s recommendations.
Preventing anal fistulas begins with addressing underlying conditions and maintaining good hygiene. If you experience any symptoms or have concerns about your risk factors, consult a proctologist immediately.
Your proactive approach can significantly impact your health outcomes. Let this knowledge empower you to take charge of your health and seek the necessary care without delay.
Ask Dr. Rajarshi Mitra
What are the common symptoms of an anal fistula?
Common symptoms include persistent pain, swelling around the anus, discharge of pus or blood, irritation of the skin around the anus, and recurrent anal abscesses.
How can I tell if I need to seek medical advice for an anal fistula?
If you experience symptoms such as unexplained anal pain, discharge, fever, or recurring abscesses near the anus, it’s crucial to consult a healthcare professional promptly.
What causes an anal fistula to develop?
Anal fistulas often result from an infection in the anal gland that leads to an abscess and subsequently creates a tunnel connecting the infected gland to the skin around the anus.
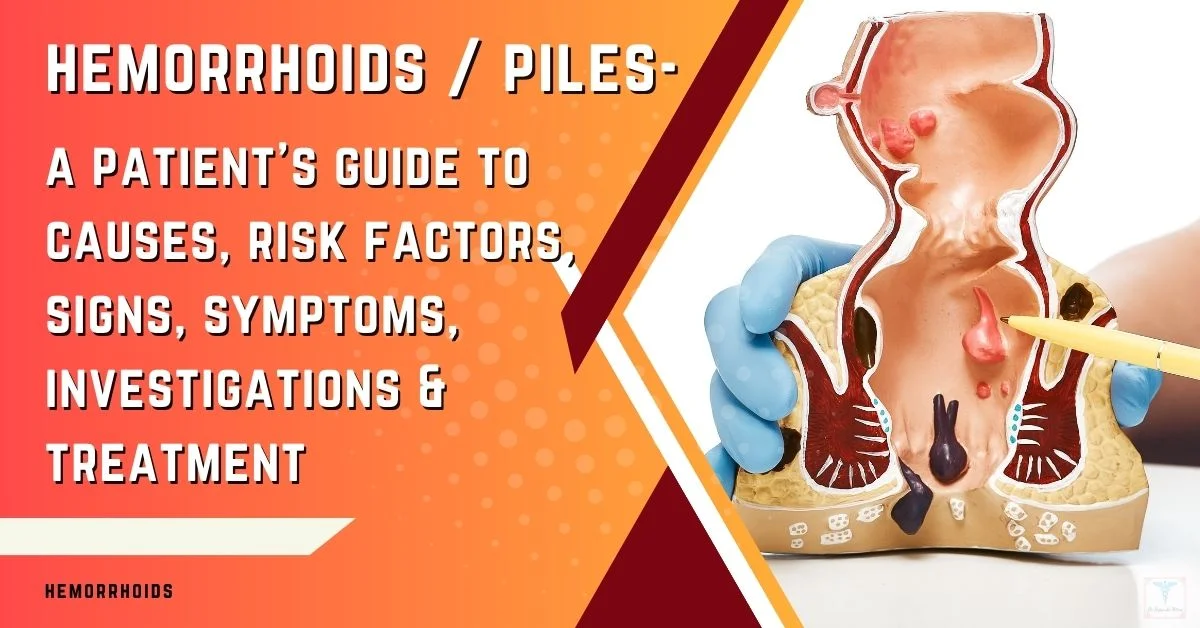
How are anal fistulas different from other anal conditions?
Anal fistulas are characterized by their tunnel-like structure connecting an internal opening within the anal canal to an external opening in the skin near the anus. This differentiates them from conditions like hemorrhoids or fissures, which don’t create such tunnels.
What treatment options are available for anal fistulas?
Treatment typically involves surgery to open and drain the fistula. Depending on its complexity, options may include a fistulotomy, seton placement, or advancement flap procedures.
What are the risks associated with surgery for an anal fistula?
Surgical risks include infection, recurrence of the fistula, incontinence (if muscles controlling bowel movements are affected), and bleeding.
How long is the recovery process after surgery for an anal fistula?
Recovery time varies but generally spans several weeks. During this period, patients may need pain management and wound care. Following post-operative instructions closely is vital for successful healing.
Can anal fistulas be prevented?
While not all cases are preventable, reducing risk factors such as treating gastrointestinal infections promptly and maintaining good hygiene can help lower your risk of developing an anal fistula.