Understanding the causes of anal fistula is crucial for those experiencing this uncomfortable condition. An anal fistula, a small tunnel connecting an abscess, a pocket of infection in the anus, to an opening on the skin around the anus, results from various factors, including infection, surgery complications, or conditions like Crohn’s disease.
Recognizing these causes can guide you toward effective treatment options and preventative measures. This guide aims to shed light on these triggers, empowering you with the knowledge to address and manage symptoms effectively.
Cause Of Anal Fistula: Quick Facts
- Understanding the causes of anal fistulas is crucial for effective prevention and management. Risk factors include previous anal abscesses, certain chronic digestive disorders like Crohn’s disease, and a history of surgery in the anal area.
- Identifying the type of anal fistula you have is a vital step towards receiving the correct treatment. Different types require different surgical interventions.
- Surgical intervention is often necessary to treat anal fistulas, with various techniques available depending on the complexity of the case. Consulting with a specialist to understand the best approach for your situation is important.
- Managing complex anal fistula cases may require a combination of surgery and other treatments. Patient-specific strategies are essential for successful outcomes.
- The recovery process post-surgery can vary; following your doctor’s advice on care and lifestyle adjustments can significantly impact your healing journey.
- Preventive measures, including addressing risk factors early and maintaining good hygiene practices, can help reduce the likelihood of developing anal fistulas.
Anal Fistula Overview
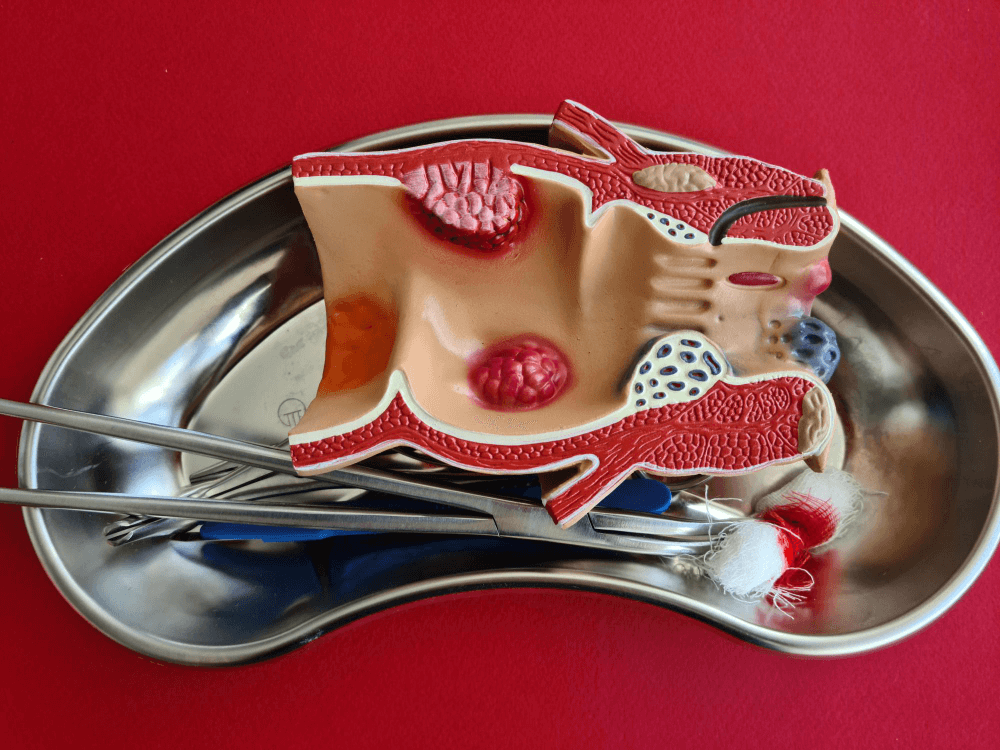
Anatomy of the Anal Canal
The anatomy of your anal canal makes it prone to infections, potentially leading to fistulas.
The structure of anal glands, in particular, can harbor infections that don’t heal properly. This can cause a persistent problem known as an anal fistula.
Anal sphincters play a crucial role in maintaining continence. However, fistulas can compromise their function, making bowel movement control challenging.
Causes of Anal Fistula
- InfectionsCommon bacteria found in the intestinal tract are often responsible for infections leading to anal fistulas. An untreated infection in an anal gland can escalate into an abscess and eventually form a fistula if not addressed promptly. Early treatment of these infections is vital to prevent the development of a fistula.
- Surgery ImpactSurgeries around the rectal or anal area might inadvertently cause fistulas. Certain procedures are more likely to result in post-operative fistulas than others. Recognizing this risk underscores the importance of post-surgery follow-ups to identify and treat potential issues early on.
- Functional AspectsAnal fistulas can disrupt regular bowel movements and lead to discomfort. They may also impact the function of anal sphincters, raising the risk of incontinence. While awaiting treatment, managing symptoms and striving to maintain anal function becomes crucial.
Risk Factors Identified
Lifestyle Influences
Your daily habits play a significant role in your health, including the risk of developing an anal fistula. Chronic constipation and straining during bowel movements can greatly increase this risk. The excessive force can cause tears and subsequent infections that may lead to fistulas.
Good hygiene practices are crucial in preventing infections around the anal area. Neglecting cleanliness can create a breeding ground for bacteria, escalating the likelihood of fistula formation.
Sexual practices also influence your risk, especially those that increase the chance of sexually transmitted infections (STIs). These infections can contribute to the development of STI-related fistulas, emphasizing the importance of safe sexual behaviors.
Medical Conditions
Crohn’s Disease
Crohn’s disease is a key medical condition linked to anal fistulas due to its inflammatory nature. This inflammation often extends to the anal region, creating pathways that can evolve into fistulas.
Managing these fistulas in Crohn’s patients presents unique challenges, requiring specialized treatment options that address both the inflammation and the presence of fistulas.
Diverticulitis
Similarly, diverticulitis increases your risk for anal fistulas. This condition causes inflammation and small pouches in your digestive tract, leading to infection and, eventually, fistula formation.
But Diverticulitis usually causes Internal Fistulas like Colo-Vesical and Recto-Vaginal Fistula. Effective management of diverticulitis is essential not only for your overall health but also for preventing complications like anal fistulas.
Understanding Fistula Relationships

Internal Opening
Fistulas create unwanted tunnels between the anal gland and the skin outside your anus. This internal connection is crucial for understanding how fistulas impact your body. Identifying the internal opening of a fistula is key to effective treatment.
Without pinpointing this opening, treatments may not reach the root cause.
Diagnostic techniques like MRI or ultrasound help map the internal pathway of a fistula. These methods provide a clear picture of how deep and complex the tunnel is, which helps doctors plan the best treatment approach.
External Opening
The external opening of a fistula can lead to significant discomfort and hygiene challenges. It’s an unwelcome gateway that allows bacteria to enter, increasing infection risk. Keeping this area clean is vital to prevent further complications.
Treatment methods focus on closing this external opening to heal the fistula completely. Techniques vary but often include surgery to ensure both ends of the fistula are addressed.
Healing from the outside prevents recurrence and promotes better health outcomes.
Types of Anal Fistulas
Simple Fistulas
Simple fistulas are less complicated than their complex counterparts. They usually have a single track and don’t involve significant parts of the anal sphincter muscles. Compared to complex fistulas, these are easier to treat.
Treatment for simple fistulas often involves less invasive methods. These can include fistulotomy, where the fistula tract is cut open and allowed to heal from the inside out. Seton techniques, involving a thread pulled through the tract to help it drain and heal over time, may also be used.
Patients with simple fistulas generally have a good prognosis after receiving proper treatment. Most experience complete healing, and their risk of recurrence is low.
Complex Fistulas
Complex fistulas are more severe and often linked to underlying diseases like Crohn’s disease. They might have multiple tracts or involve a significant portion of the sphincter muscles, making treatment challenging.
Treating complex fistulas typically requires more specialized surgical techniques. These can include advanced seton placement, fibrin glue injection, or even rectal advancement flap procedures.
Due to their complexity, these treatments require careful planning and execution by an experienced proctologist and surgeon.
A multidisciplinary approach is crucial for managing patients with complex fistulas. This includes gastroenterologists, proctologists, and sometimes radiologists working together to provide comprehensive care.
Surgical Intervention Insights
Procedure Overview
Surgical methods like fistulotomy and seton placement are common for treating anal fistulas. Doctors choose a method based on the fistula type and your health. Each option has its risks and benefits.
Fistulotomy involves cutting open the whole length of the fistula to flush out content. It’s effective but might not suit complex cases.
Seton placement uses a thread to keep the fistula open, allowing it to drain over time. This method reduces infection risks but takes longer to heal.
Risks Involved
- Risk of InfectionExisting infections complicate anal fistula treatment. To lower post-surgery infection risks, doctors take preventive measures. They might prescribe antibiotics before and after surgery. Cleanliness around the surgical area is crucial, too.
- Likelihood of RecurrenceSome factors increase the chance of an anal fistula coming back after treatment. These include the type of fistula and how well you follow post-surgery care instructions. Eating right and staying active can help reduce recurrence risks. Regular check-ups allow early detection and treatment of any signs of return.
Managing Complex Cases
Advanced Surgical Techniques
Advances in medical science have introduced newer surgical techniques for treating anal fistulas. Among these, Obsidian Regenerative Treatment, laser therapy, and video-assisted anal fistula treatment (VAAFT) stand out.
These methods offer significant benefits over traditional surgery. They often result in reduced recovery time and lower recurrence rates.
It is crucial to consult with a specialist experienced in these advanced treatments. Their expertise can ensure the most effective management of complex anal fistula cases.
Post-Surgery Care
Proper care is essential for healing and preventing infection after surgery. You should closely follow your doctor’s instructions on wound care and activity restrictions. This might include keeping the area clean and avoiding strenuous activities.
Be vigilant for signs of complications, such as increased pain or unusual discharge from the wound site. These symptoms require immediate medical attention to prevent further issues.
Recovery Process Explained

Healing Time
After undergoing surgery for an anal fistula, your body needs time to heal. Typically, the healing process can span from a few weeks to several months.
The recovery speed varies depending on your overall health and the complexity of the fistula. For instance, a straightforward fistula might heal faster than one that is complex or involves multiple tracts.
It’s crucial to understand that healing takes time. Patience and closely following post-surgery guidelines are key to optimal healing. Your doctor will provide specific instructions tailored to your case. Adhering to these can significantly influence the recovery timeline.
Lifestyle Adjustments
Certain lifestyle adjustments are beneficial to support your healing journey and prevent future occurrences. Increasing fiber intake and staying well-hydrated help maintain regular bowel movements, reducing strain on the anal area.
Regular exercise and maintaining a healthy weight contribute to overall good health, which can expedite the healing process.
During recovery, it’s important to avoid activities that put excessive strain on the anal area. This precaution helps prevent complications and supports smoother healing.
Embracing these lifestyle changes not only aids in your current recovery but also plays a role in preventing future anal fistulas.
Preventive Measures
Diet Recommendations
To support your recovery from an anal fistula, adjusting your diet is crucial. You should focus on high-fiber foods such as fruits, vegetables, and whole grains.
These help ease bowel movements and can significantly aid in the healing process. Alongside fiber, ensure you drink plenty of fluids to avoid constipation, which can strain the affected area.
On the flip side, some foods might worsen your condition. Spicy foods, dairy products, and those high in fat should be limited.
They can irritate your digestive system and delay healing. Remember, a balanced diet not only aids in preventing anal fistulas but also bolsters your overall health.
Regular Check-ups
After undergoing treatment for an anal fistula, regular follow-ups with your healthcare provider are essential. These check-ups allow for monitoring of the healing process and early detection of any recurrence.
During these appointments, you may undergo examinations or tests to assess the state of your recovery.
Ongoing medical supervision is critical in managing your long-term health and preventing complications. It ensures that any issues are caught early and addressed promptly. Therefore, never skip these important visits to your healthcare provider.
Final Note From Dr. Rajarshi Mitra
Understanding the causes and management of anal fistulas is crucial for effective treatment and recovery. We have already explored the overview, risk factors, relationships, types, surgical interventions, management of complex cases, recovery processes, and preventive measures related to anal fistulas.
You’ve gained insights into how these factors interplay to influence the condition’s onset and progression. It’s essential to recognize symptoms early and consult healthcare professionals for diagnosis and treatment options tailored to your specific situation.
Preventive measures can significantly reduce the risk of developing an anal fistula. However, if you find yourself facing this condition, remember that advancements in medical science offer effective solutions for managing even the most complex cases.
Stay informed about your health options and take proactive steps toward your well-being. We encourage you to share this knowledge with others who might benefit from it and continue exploring this topic through reputable sources.
Ask Dr. Rajarshi Mitra
What causes an anal fistula?
Anal fistulas commonly result from an infection in the anal gland that leads to a chronic abscess, eventually forming a fistula.
Can certain conditions increase the risk of developing an anal fistula?
Yes, conditions like Crohn’s disease, previous surgery near the anus, and a history of abscesses can elevate the risk of anal fistulas.
Are there different types of anal fistulas?
Indeed, anal fistulas are classified into four main types: inter-sphincteric, trans-sphincteric, supra-sphincteric, and extra-sphincteric, based on their relation to the sphincter muscles.
What are common surgical options for treating an anal fistula?
Surgical treatments include fistulotomy, seton placement, and advanced procedures like LIFT (ligation of intersphincteric fistula tract) or flap procedures for complex cases.
How long is the recovery process after anal fistula surgery?
Recovery time varies but generally takes several weeks. Patients must follow post-operative care instructions carefully to aid healing.
What measures can help prevent an anal fistula?
Preventive measures include maintaining good hygiene, treating gastrointestinal infections promptly, and managing conditions like Crohn’s disease effectively to reduce infection risks.