An anal fissure is a small tear in the lining of the anus that can cause discomfort during bowel movements. In this blog, we discuss the symptoms and causes of anal fissures, as well as ways to prevent and treat this common condition. Read about anal fissures to learn more and find relief.
- BOOK A CONSULTATION WITH Dr. RAJARSHI MITRA
- WHAT IS AN ANAL FISSURE?
- WHAT ARE THE CAUSES OF ANAL FISSURE?
- WHAT ARE THE RISK FACTORS FOR ANAL FISSURE?
- TYPES OF ANAL FISSURE
- WHAT ARE THE SYMPTOMS OF ANAL FISSURE?
- WHAT ARE THE SIGNS OF ANAL FISSURE ON PHYSICAL EXAMINATION?
- WHAT ARE THE TREATMENT OPTIONS FOR ANAL FISSURE?
- WHAT ARE THE MEDICAL TREATMENT FOR ANAL FISSURE?
- WHAT ARE THE SURGICAL TREATMENTS FOR ANAL FISSURE?
- WHAT IS THE POST OPERATIVE CARE FOLLOWING SURGERY FOR ANAL FISSURE?
- PAIN MANAGEMENT FOR ANAL FISSURE
- HOME REMEDIES FOR ANAL FISSURE
- DIET & NUTRITION FOR ANAL FISSURE
- PREVENTION OF ANAL FISSURE- HOW CAN I PREVENT ANAL FISSURES?
- ROLE OF BOTOX IN THE MANAGEMENT OF ANAL FISSURE
- CONCLUSION
- IMPORTANT NOTE & DISCLAIMER
Quick Synopsis: In a hurry? Read through this quick summary of Anal Fissure, its causes, risk factors, types, and treatment.
What is Anal Fissure?
An Anal Fissure, also known as Fissure-in-Ano, is a small tear or cut in the thin skin lining the external opening of the anal canal.
What are the common causes of Anal Fissure?
Passing Hard Stools.
Passing large amount of stool suddenly.
Persistent watery stools or diarrhea.
During childbirth.
Anal Intercourse.
Inflammatory Bowel Disease like Chron’s Disease.
Syphilis.
Tuberculosis.
HIV.
Anal Cancer.
What are the Risk Factors of Anal Fissure?
Injury to the anal mucosa can happen when:
- You pass a large and hard stool
- You are constipated and try to pass a hard stool
- You have repeated diarrhea
- You gave birth (childbirth can cause trauma to anal canal)
- Any foreign body entering into the anal canal
- In some cases, due to Crohn’s disease
What are the Types of Anal Fissure?
Anal Fissure are usually of Two Types:
- Acute Anal Fissure: Anal Fissures of Recent Onset.
- Chronic Anal Fissure: Anal Fissures lasting for more than 8 to 12 weeks.
What are the Symptoms of Anal Fissure?
Symptoms of anal fissure may include:
Pain, sometimes severe, during bowel movement.
Burning or Itching sensation in the anal canal.
You may see a small spot of bright red blood on toilet paper or a few drops in the toiled bowel.
A visible crack in the skin around the anus.
A small lump or skin tag on the skin near the anal fissure.
What are the Signs of Anal Fissure?
- Looking at the fissure by gently separating the buttocks.
- A digital rectal examination, in which the doctor inserts a gloved finger into the anal canal.
- Initially, a fissure is just a tear in the anal mucosa and is defined as an acute anal fissure. If the fissure persist over time, it progresses to chronic fissure, and often, an enlarged anal skin tag is present in the anal canal proximal to the fissure and hypertrophied anal papillae are present in anal canal proximal to fissure.
- Most anal fissures occur in the posterior midline, with remainder occurring in the anterior midline. About 2% of the patients have anterior and posterior fissures.
- Fissures occurring off the midline should raise the possibility of other bowel conditions (for example Crohn’s disease), infection (for example sexually transmitted diseases or AIDS), or cancer.
- Anoscopy: This involves using a short, lighted scope to look into the canal.
What are the Treatment Options for Anal Fissure?
Majority of the Anal Fissures will not need any surgical treatment.
Lifestyle modifications like High Fibre Diet, Stool Softeners, Increasing water intake to promote soft bowel movements, Warm Sitz Bath, Local application of appropriate ointments will usually promote the healing of the Anal Fissure.
Chronic Anal Fissures and very rarely certain Acute Anal Fissures not responding to medical therapy, will need Surgical Treatment.
What are the Medical Treatment for Anal Fissure?
First line of treatment consists of therapy with stool-bulking agents, such as fiber supplementation and stool softeners.
Laxatives are used as needed. Mineral oil may be added to facilitate the passage of stool.
Sitz baths after bowel movements and as needed to provide significant symptomatic relief.
Second line medical therapy consists of intra-anal application of 0.4% nitroglycerin (NTG; also called glycerol trinitrate) ointment directly to internal sphincter.
What are the Surgical Treatment for Anal Fissure?
The most commonly performed surgery is a Lateral Internal Sphincterotomy.
Certain Chronic Fissure which may not heal completely with a Lateral Sphincterotomy, will need an Excision of the Fissure with cover of the defect by an Advancement Flap.
Lasers can be also used as a modality in the treatment of Anal Fissure.
What Post Operative Care is required after Anal Fissure Surgery?
- Try to avoid constipation
- Include fruit, vegetables, beans, and whole grains in your diet every day. These foods are higher in fiber.
- Drink plenty of fluids.
- Get some exercise every day.
- Take a fiber supplement, every day if needed.
- Do not strain when you have bowel movement and do not sit on toilet too long.
- Take Sitz baths 2 to 3 three times every day.
- Instead of using toilet paper, use baby wipes or medicated pads.
BOOK A CONSULTATION WITH Dr. RAJARSHI MITRA
Reach out to Dr Rajarshi Mitra Today, to:
- Understand your Surgical Issue.
- Discuss various Treatment Options.
- Get a Second Opinion.
- Advice on Post Operative Care.

NB: Due to his busy surgical practice, Dr. Rajarshi Mitra accepts very limited appointments for Online Consultations.
WHAT IS AN ANAL FISSURE?
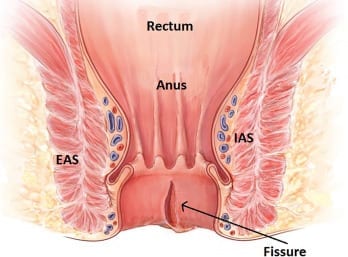
An anal fissure is a small tear in the lining of the anal canal. It is a common condition that causes pain, burning, and bleeding during bowel movements.
Anal fissures typically occur when there is an increase in pressure on the anus, such as during hard stools or constipation. They can also be caused by childbirth and other types of trauma to that area.
Symptoms of an anal fissure include severe pain and itching around the anus, bright red blood on the toilet paper after a bowel movement, and a visible tear or crack in the skin near the opening of the anus.
Treatment for an anal fissure usually involves keeping the area clean and applying topical medications to reduce pain and inflammation, which may allow the fissure to heal within the anal canal.
In some cases, surgery may be necessary to repair the tear if it does not heal on its own.
An Anal Fissure is also known as Fissure-in-Ano.
Initially, it usually involves only epithelium, but if left untreated involves the total thickness of the anal mucosa. The tear in the anal canal leads to a reduction in the blood flow to that area which further impedes the ability of the fissure to heal.
Anal fissures develop with equal frequency in both sexes; they tend to occur in younger and middle-aged persons.
WHAT ARE THE CAUSES OF ANAL FISSURE?

Anal fissures are quite common and uncomfortable condition that affects the area around the anus. The fissure is a small tear or cut in the skin that can be either acute or chronic.
- The most common cause of anal fissures is constipation and straining during bowel movements. This causes the anal sphincter muscle to become tight and overstretched, leading to a tear.
- Other causes can include childbirth, diarrhea, and inflammatory bowel disease.
- In some cases, an underlying infection may cause an anal fissure. This can happen when the infected tissue is exposed to air and irritated.
- Anal fissures can also occur as a result of an abnormal growth or tumor in the anal canal or as a result of Crohn’s disease or other inflammatory bowel diseases.
- In rare cases, an anal fissure may be caused by an injury or trauma to the area. This can occur during certain activities such as cycling, horseback riding, or sexual intercourse.
- Anal fissures can also be caused by using certain medications, such as those used to treat Crohn’s disease or ulcerative colitis.
- In some cases, radiation therapy used to treat cancer may also be a contributing factor.
Regardless of the cause, anal fissures can be painful and uncomfortable. If you experience any pain or discomfort in the anal region, you must see a doctor to determine the underlying cause and get the appropriate treatment.
SUMMARY BOX:
To Summarize, Common Causes of Anal Fissures:
1. Constipation and straining during bowel movements are the most common cause of anal fissures.
2. Other causes can include childbirth, diarrhea, and inflammatory bowel disease.
3. An underlying infection may be the cause of an anal fissure.
4. Anal fissures can also occur as a result of an abnormal growth or tumor in the anal canal or as a result of Crohn’s disease or other inflammatory bowel diseases.
5. In rare cases, an anal fissure may be caused by an injury or trauma to the area, like anal intercourse.
6. Certain medications, such as those used to treat Crohn’s disease or ulcerative colitis, can also cause anal fissures.
7. Radiation therapy used to treat cancer may also be a contributing factor.
Less Common Causes of Anal Fissures:
Syphilis.
Tuberculosis.
HIV.
Anal Cancer.
WHAT ARE THE RISK FACTORS FOR ANAL FISSURE?

Injury to the anal mucosa can happen when:
- You pass a large and hard stool
- You are constipated and try to pass a hard stool
- You have repeated diarrhea
- You gave birth (childbirth can cause trauma to anal canal)
- Any foreign body entering into the anal canal
- In some cases, due to Crohn’s disease
TYPES OF ANAL FISSURE

Anal Fissure are usually of Two Types:
- Acute Anal Fissure: Anal Fissures of Recent Onset.
- Chronic Anal Fissure: Anal Fissures lasting for more than 8 to 12 weeks.
Location of Anal Fissure:
Most Anal Fissures, about 85%-90% are located in the Posterior Midline or 6 O’ clock position.
About 10%-15% are located in the Anterior Midline or 12 O’ clock position.
Few patients will have fissure in both 6 & 12 O’ clock position.
Fissures which are located off the midline, to the sides, should raise suspicion of some other underlying disease and should be investigated further.
WHAT ARE THE SYMPTOMS OF ANAL FISSURE?
Anal fissures are small tears or cuts in the lining of the anus, often caused by straining during a bowel movement. Anal Fissures typically cause severe pain and bleeding with bowel movements.
Symptoms of an anal fissure can range from mild to severe and can include the following:
•Pain during bowel movements. The pain can be sharp, burning, or tearing, and may last several hours after a bowel movement.
•Bright red blood on the stool, toilet paper, or drops in the toilet bowel. The blood from the fissure is separate from the stool.
•Burning or Itching sensation in the anal canal or irritation around the anus can sometimes last for quite some time after passing stools.
•A visible tear or crack in the skin around the anus.
•A small lump or skin tag on the skin near the anal fissure
•A feeling of incomplete bowel movements.
Sometimes, an anal fissure may be a painless wound that won’t heal. It may bleed from time to time but cause no other problem.
In addition to the symptoms and signs mentioned above, some people with an anal fissure may experience spasms in the anal muscles.
These spasms can cause pain and make it difficult to have a bowel movement.
Some people also experience discomfort in the area around the anus and may feel the need to constantly scratch or rub the area.
An anal fissure can cause a fever, chills, or even severe pain in more severe cases. If the fissure grows deep enough, it can cause a discharge of pus or blood. If the fissure becomes infected, it can lead to abscesses in the area.
If you are experiencing any of these symptoms or signs, it is essential to contact your doctor as soon as possible. Anal fissures can often be treated with simple lifestyle changes, medications, or surgery. Early diagnosis and treatment can help prevent the fissure from worsening and causing further complications.
SUMMARY BOX:
To Summarize, the Symptoms of Anal Fissures:
- Pain during Bowel Movements.
- Bright Red Blood on the stool.
- Burning or Itching sensation after passing stools.
- A visible crack in the skin of the anus.
- A small lump or skin tag near the anal verge.
- Spasm of the anal muscles.
- Feeling of incomplete bowel evacuation.
- Rarely an Abscess, secondary to infection.
WHAT ARE THE SIGNS OF ANAL FISSURE ON PHYSICAL EXAMINATION?

A doctor can diagnose an anal fissure based on your symptoms and a physical examination. The examination may include:
- Looking at the fissure by gently separating the buttocks.
- A digital rectal examination, in which the doctor inserts a gloved finger into the anal canal.
- Initially, a fissure is just a tear in the anal mucosa and is defined as an acute anal fissure. If the fissure persist over time, it progresses to chronic fissure, and often, an enlarged anal skin tag is present in the anal canal proximal to the fissure and hypertrophied anal papillae are present in anal canal proximal to fissure.
- Most anal fissures occur in the posterior midline, with remainder occurring in the anterior midline. About 2% of the patients have anterior and posterior fissures.
- Fissures occurring off the midline should raise the possibility of other bowel conditions (for example Crohn’s disease), infection (for example sexually transmitted diseases or AIDS), or cancer.
- Anoscopy: This involves using a short, lighted scope to look into the canal.
WHAT ARE THE TREATMENT OPTIONS FOR ANAL FISSURE?

Majority of the Anal Fissures will not need any surgical treatment.
Lifestyle modifications like High Fibre Diet, Stool Softeners, Increasing water intake to promote soft bowel movements, Warm Sitz Bath, Local application of appropriate ointments will usually promote the healing of the Anal Fissure.
Chronic Anal Fissures and very rarely certain Acute Anal Fissures not responding to medical therapy, will need surgical treatment.
WHAT ARE THE MEDICAL TREATMENT FOR ANAL FISSURE?

Initial therapy for an anal fissure is medical in nature, and more than 80% of acute anal fissures resolve without further therapy. The treatment goals are to relieve constipation and to break the cycle of hard bowel movement, associated pain, and worsening constipation. Softer bowel movements are more manageable and less painful for the patient to pass.
The first line of treatment consists of therapy with stool-bulking agents, such as fiber supplementation and stool softeners.
Laxatives are used as needed. Mineral oil may be added to facilitate the passage of stool.
Sitz baths after bowel movements and as needed to provide significant symptomatic relief.
Second line medical therapy consists of intra-anal application of 0.4% nitroglycerin (NTG; also called glycerol trinitrate) ointment directly to the internal sphincter.
NTG is approved by US food and drug administration (FDA) for moderate to severe pain associated with anal fissures and may be considered when conservative therapies have failed.
WHAT ARE THE SURGICAL TREATMENTS FOR ANAL FISSURE?

There are various Surgical Treatment options for Anal Fissure.
The most commonly performed surgery is a Lateral Internal Sphincterotomy, which cuts a portion of the Internal anal sphincter and can relax the anal sphincter.

Particular Chronic Fissures which may not heal entirely with a Lateral Sphincterotomy will need an Excision of the Fissure with a cover of the defect by an Advancement Flap.
The edges of the fissure along with the underlying unhealthy tissue are all excised.
This is done to ensure that the fissure has healed properly and does not result in any narrowing of the anal canal opening.
LASERS IN THE TREATMENT OF ANAL FISSURE:
Lasers can also be used as a modality in treating Acute Anal fissures.
SUMMARY BOX:
To Summarize, the TREATMENT OPTIONS for Anal Fissures:
MEDICAL MANAGEMENT:
- Fibre Supplements.
- Stool Softeners.
- Laxatives.
- Sitz Bath.
- Anti-Inflammatory Medications.
- NTG Ointment.
- Diltiazem Ointment.
SURGICAL MANAGEMENT:
- Lateral Internal Sphincterotomy.
- Fissurectomy with Flap Cover.
- Lasers.
WHAT IS THE POST OPERATIVE CARE FOLLOWING SURGERY FOR ANAL FISSURE?

- Try to avoid constipation
- Include fruit, vegetables, beans, and whole grains in your diet every day. These foods are higher in fiber.
- Drink plenty of fluids.
- Get some exercise every day.
- Take a fiber supplement, every day if needed.
- Do not strain when you have bowel movement and do not sit on toilet too long.
- Take Sitz baths 2 to 3 three times every day.
- Instead of using toilet paper, use baby wipes or medicated pads.
PAIN MANAGEMENT FOR ANAL FISSURE
 Pain management is an essential component of treatment for anal fissures.
Pain management is an essential component of treatment for anal fissures.
Anal fissures can be very painful, and the pain can be challenging to manage.
Fortunately, several treatment options are available to help reduce pain and discomfort associated with anal fissures.
- A topical anesthetic ointment is one of the most common treatments for anal fissures. These ointments can be applied directly to the affected area to help numb the area and reduce pain.
- Another option is to use a topical corticosteroid cream. These creams can reduce inflammation and help reduce pain.
- In addition to topical treatments, some people may find pain relief from taking over-the-counter pain medications, such as ibuprofen or acetaminophen. However, speaking to your doctor before taking any medication is essential, as some medicines may not be safe for everyone.
- Dietary modifications can also help manage anal fissure pain.
- Eating a high-fiber diet can help reduce bowel movements’ frequency, reducing the amount of pain associated with passing stool.
- It is also essential to stay hydrated by drinking plenty of water. This can help soften stool and make it easier to pass.
- Finally, relaxation techniques can help reduce the pain associated with anal fissures.
Deep breathing, meditation, and visualization can help reduce stress and relax the muscles in the anal area. This can help reduce the pain associated with passing stool.
Overall, various treatment options are available to help manage anal fissure pain. You must speak to your doctor to determine your best treatment plan.
SUMMARY BOX:
To Summarize, the Pain Management for Anal Fissures:
- Topical Anesthetic Ointment.
- Topical Corticosteroids Ointment.
- OTC Analgesics.
- Dietary Modifications.
- High Fiber Diet.
- Staying well Hydrated.
- Relaxation Techniques.
HOME REMEDIES FOR ANAL FISSURE

Home remedies for anal fissures can be a great way to help relieve the discomfort associated with this condition.
Anal fissures can be very uncomfortable and painful, but luckily, many home remedies can provide relief.
Here are some home remedies for anal fissures:
1. Increase your water intake: Drinking plenty of water can help to soften the stool and reduce the amount of straining needed during bowel movements. This can help to reduce the risk of further tears.
2. Try a high-fiber diet: Eating high-fiber foods such as fruits, vegetables, and whole grains can help to soften the stool and reduce the strain during bowel movements.
3. Use a stool softener: Over-the-counter medications such as docusate sodium (Colace) can help to reduce the amount of straining needed during bowel movements.
4. Apply topical ointments: Over-the-counter ointments such as zinc oxide can be applied directly to the fissure to help promote healing.
5. Take a warm bath: Taking a warm bath several times a day can help to relax the sphincter muscles and reduce pain.
6. Try an over-the-counter pain relief medication: Acetaminophen or ibuprofen can help to reduce pain and inflammation.
7. Avoid straining: Straining during bowel movements can put extra pressure on the anal canal and make anal fissures worse.
8. Use a Squatty Potty: This device helps to reduce straining by positioning the body in a squatting position while on the toilet.
9. Try a topical anesthetic: Over-the-counter topical anesthetics such as lidocaine can help to reduce pain.
10. Adding probiotics to your diet may help reduce inflammation and promote the healing of your anal fissure.
While home remedies can be beneficial in some cases, it’s essential to consult your doctor if your symptoms persist or worsen over time.
SUMMARY BOX:
10 Home Remedies for Anal Fissures:
1. Increase your water intake.
2. Try a high-fiber diet.
3. Use a stool softener.
4. Apply topical ointments.
5. Take a warm bath.
6. Try an over-the-counter pain relief medication.
7. Avoid straining.
8. Use a Squatty Potty.
9. Try a topical anesthetic.
10. Use Probiotics.
DIET & NUTRITION FOR ANAL FISSURE

Diet and nutrition are essential in managing anal fissures and promoting healing.
Eating the right foods can help reduce the pain and discomfort caused by anal fissures and help the fissures heal.
• Consume foods that are high in fiber: Eating foods that are high in fiber, such as fruits, vegetables, and whole grains, can help promote regular and easy bowel movements, reducing the strain on the anus and helping fissures heal.
• Avoid spicy and processed foods: These foods can aggravate the area and worsen the pain of anal fissures.
• Eat plenty of protein: Protein is vital for healing and repairing tissues in the body. Eating lean meats, fish, eggs, and legumes can help the body repair the fissure.
• Consume foods rich in omega-3 fatty acids: Omega-3 fatty acids can help reduce inflammation, which can reduce the pain associated with anal fissures. Foods like fatty fish, nuts, and seeds are good sources of omega-3 fatty acids.
• Add probiotics to your diet: Probiotics are the beneficial bacteria that live in the digestive system and help maintain a healthy balance of bacteria. Probiotic-rich foods like yogurt, kefir, and sauerkraut can help reduce inflammation and improve digestive health.
• Stay hydrated: Drinking plenty of water throughout the day can help keep your stools soft and reduce the strain on the anus.
SUMMARY BOX:
Diet & Nutrition for Anal Fissures:
• Consume foods high in fiber.
• Avoid spicy and processed foods.
• Eat plenty of protein.
• Consume foods rich in omega-3 fatty acids.
• Add probiotics to your diet.
• Stay hydrated.
PREVENTION OF ANAL FISSURE- HOW CAN I PREVENT ANAL FISSURES?
Anal fissures are tears in the lining of the anus that can cause pain, itching, and bleeding.
Fortunately, there are several things you can do to prevent anal fissures.
1. Stay Hydrated: Dehydration can cause constipation, leading to the development of anal fissures. Drinking plenty of water throughout the day can help you stay hydrated and prevent constipation.
2. Eat High-Fiber Foods: Eating fiber-rich foods like vegetables, and whole grains can help prevent constipation and reduce the risk of developing anal fissures.
3. Avoid Straining: Straining during bowel movements can put too much pressure on the anus and increase the risk of anal fissures. To avoid straining, make sure to empty your bowels when you feel the urge.
4. Use Soft Toilet Paper: Avoid using scented or rough toilet paper, which can irritate the anus and make it more prone to fissures. Instead, opt for softer, unscented toilet paper.
5. Use Stool Softeners: If you are experiencing constipation, talk to your doctor about taking a stool softener to help reduce the risk of anal fissures.
6. Avoid Long Sitting Times: Sitting for long periods can put pressure on the anus, so getting up and moving around throughout the day is essential.
7. Keep the Anal Area Clean: Proper hygiene is essential for preventing anal fissures. After a bowel movement, use soft toilet paper to clean the area gently.
Preventing anal fissures requires making specific lifestyle changes.
SUMMARY BOX:
How Can I Prevent Anal Fissures:
1. Stay hydrated.
2. Eat high-fiber foods.
3. Avoid straining.
4. Use a soft toilet paper.
5. Use stool softeners.
6. Avoid long sitting times.
7. Keep the anal area clean.
ROLE OF BOTOX IN THE MANAGEMENT OF ANAL FISSURE

Anal fissures are a common problem that can cause pain and bleeding. Anal Fissure is a tear in the anal canal caused by trauma to the anus, often in the form of hard or large stools, constipation, or childbirth. This results in a tight anal sphincter and causes severe pain near the anus. The most common treatment for anal fissures is a combination of medications, lifestyle changes, and topical creams.
In some cases, Botox injections may help relax the anal muscles and reduce spasms, allowing the fissure to heal.
The role of Botox in the management of anal fissures:
- Botox injections can help relax the anal muscles and reduce spasms, allowing the fissure to heal.
- Botox is typically used when other treatments have failed or as an adjunct to other treatments.
- Botox injections are administered by a healthcare provider, typically in the office.
- Botox injections can provide temporary relief from anal spasms and pain.
- Side effects of Botox injections may include mild bleeding, bruising, and pain at the injection site.
- Botox injections should not be used in patients with specific conditions such as bleeding disorders or infections.
CONCLUSION
In conclusion, anal fissures are common and are caused by damage to the skin around the anus.
Most people will experience pain and spasms in this area at some point in their life. Everyone will need some or other form of treatment.
Diagnosis and treatment of anal fissures typically involve a combination of diet and lifestyle changes and medical interventions.
Changing your diet and lifestyle can help improve anal fissures, but in some cases, further treatment may be necessary if the fissure fails to heal or does not heal completely.
It is essential to consult with a healthcare provider for proper diagnosis and treatment to ensure that the fissure heals appropriately.
Anal fissures can be uncomfortable and painful, but most fissures will heal completely with proper treatment.
It is essential to follow your healthcare provider’s treatment recommendations and make any necessary changes to your diet and lifestyle to promote healing.
If the fissure fails to heal or does not heal completely, further treatment may be necessary.
Surgery may sometimes be required to repair the damaged tissue and promote healing.
By seeking proper diagnosis and treatment, you can help to ensure that your anal fissure heals appropriately and does not cause further discomfort or complications.
IMPORTANT NOTE & DISCLAIMER
This article is only for informational purpose and is NOT a substitute for an actual consultation with your Surgeon or GP.As always, please consult your doctor, talk about the various treatment options for your medical issue, and make a decision.