As the new year unfolds like a blank page ready for fresh stories, you may find yourself reflecting on your health and well-being. Among the myriad of resolutions, consider turning attention to a common yet often overlooked issue: healing anal fissures.
You’re not alone if you’ve experienced the discomfort and inconvenience they bring. While the topic might be uncomfortable to discuss, understanding the importance of addressing anal fissures is crucial for your overall health.
Implementing simple lifestyle changes and exploring treatment options can significantly alleviate symptoms and promote healing. So, what are the steps you can take to ensure these painful interruptions don’t overshadow your plans for a healthier year?
Stay with us as we explore the paths to not just managing but overcoming this delicate health challenge.
Healing Anal Fissures: Key Takeaways
- Anal fissures can be acute or chronic, and chronic fissures may require longer healing time.
- Modifying bowel habits, increasing fiber intake, and taking warm baths can help alleviate symptoms and promote healing.
- Symptoms of anal fissures include sharp pain during bowel movements, fresh blood on the stool or toilet paper, and a burning sensation or itchiness in the anal area.
- Early detection and treatment can prevent the progression of acute fissures to chronic fissures.
Understanding Anal Fissures
Anal fissures, often resulting from excessive strain during bowel movements or other stressors on the anal canal, are painful tears in the mucosal lining that can cause significant discomfort and bleeding.
When you’re facing a sharp sting or throbbing ache in your anal region, it’s likely due to these small yet distressing splits, which can be acute or develop into chronic anal fissures if not addressed properly.
Chronic anal fissures persist longer and may not heal within the typical few weeks due to ongoing tension in the anal muscles, particularly the internal sphincter. This involuntary muscle, responsible for maintaining continence, can spasm and exacerbate the problem, hindering the healing process and intensifying pain.
To achieve pain relief and facilitate healing, it’s crucial to modify your bowel habits. Increasing your intake of fiber supplements and ensuring adequate hydration can soften stools, reducing the need to strain.
Warm baths can also soothe the anal canal, promoting relaxation of the sphincter muscles.
If you’re noticing blood during bowel movements, or if discomfort persists, seek medical evaluation. Your healthcare provider can confirm the presence of an anal fissure and offer comprehensive treatment options tailored to your specific needs. Remember, you don’t have to suffer in silence; effective help is available.
Identifying Symptoms and Causes
Recognizing the symptoms and understanding the diverse causes of anal fissures is a crucial step towards effective treatment and relief.
As you navigate this health challenge, it’s essential to be aware of the signs that indicate an anal fissure and the factors that may contribute to its development.
- Symptoms of an Anal Fissure1. Sharp pain during bowel movements that may persist afterwards.
2. Fresh, red blood on the stool or toilet paper, signaling pain and bleeding.
3. A burning sensation or itchiness in the anal area. - Common Causes1. Straining to pass hard bowel movements, often due to chronic constipation.
2. Childbirth or other forms of trauma to the anal canal.
3. Diseases such as inflammatory bowel disease, which can compromise blood flow and tissue integrity. - Chronic FissuresIf healing is delayed, anal fissures can become chronic, causing ongoing pain and prompting the anal sphincter to clench, further reducing blood flow and impeding recovery.
Seeking symptoms and help early can prevent the progression of chronic anal fissures. Your sense of belonging in a community focused on health and well-being is supported as you take informed steps to address anal fissure issues.
Exploring Diagnosis and Tests
Understanding the symptoms of anal fissures paves the way for accurate diagnosis, which healthcare providers typically perform through a detailed physical examination and specific tests. Chronic anal fissures, which are persistent tears in the lining of the anus, can be differentiated from acute anal fissures by their duration and severity.
Your healthcare provider will carefully assess your symptoms, which may include pain during bowel movements and visible tears around the anus.
During a physical examination, the provider may gently separate your buttocks to check for tenderness or muscle spasms. This step is crucial in identifying the presence of a fissure.
In some cases, a digital rectal exam is warranted to explore the anal canal in more detail, ensuring no underlying issues such as inflammatory bowel disease are contributing to your condition.
Tests to detect blood in the stool can also support the diagnosis, indicating whether there’s ongoing bleeding associated with the fissure.
Your personal health history and an accurate description of your symptoms are vital in guiding the healthcare provider towards the appropriate medical treatments, which may include stool softeners to ease strain, measures for relaxing the anal sphincter to allow blood to flow more freely, and other therapeutic interventions.

Effective Treatment Options
To effectively treat anal fissures, incorporating lifestyle changes and medical interventions is essential for promoting healing and preventing recurrence. It’s about taking control of your body and finding relief. Here’s a clear path forward:
- Warm Sitz BathsImmerse yourself in warm water several times a day, especially after going to the bathroom. This simple act can relax your sphincter muscle, improve blood flow to the area, and aid in the healing process.
- Dietary AdjustmentsIncrease the amount of fiber in your diet through natural sources or supplements like psyllium. It won’t just help you today; it’ll make going to the bathroom easier in the long run. Remember, staying hydrated works hand in hand with your fiber intake to keep bowel movements soft and manageable.
- Medical and Topical TreatmentsFor chronic anal fissures, your healthcare provider may suggest topical treatments that increase blood flow and relax the sphincter muscle. If conservative measures fail, surgery might be the recommended course to heal the fissure and alleviate pain.
Countless individuals have faced and overcome the discomfort of anal fissures. With these treatments, you’re taking important steps towards your own healing and comfort.
Strategies for Prevention and Management
While effective treatment options can provide relief, implementing preventative strategies ensures long-term management and reduces the risk of recurrent anal fissures.
To maintain the healing flow, integrate hot baths into your daily routine, ideally three times a day. This practice not only relaxes your anal muscles but also promotes circulation, creating an environment that allows the fissure to mend.
You should also increase your fiber intake with raw fruits, vegetables, and fiber supplements. This dietary adjustment softens your stool, making bowel movements less traumatic and giving your body a chance to repair without re-injury. Additionally, stay hydrated by drinking plenty of fluids, which supports the healing process.
If a chronic anal fissure won’t heal after eight weeks, despite these efforts, consult your healthcare provider for further advice.
They may suggest the use of stool softeners, medicated creams, or even channel blockers, which can further alleviate symptoms and facilitate healing. In some cases, surgery might be recommended.
Final Note From Dr. Rajarshi Mitra
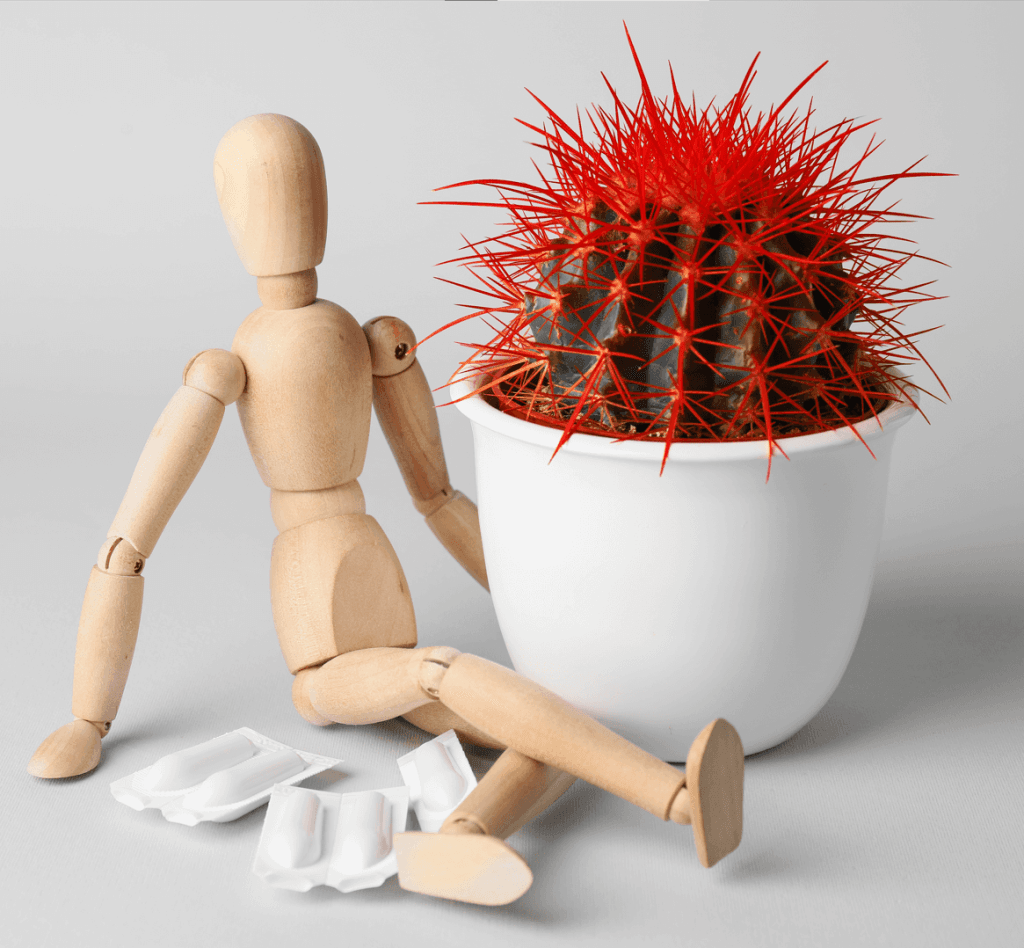
As you embark on healing your anal fissure, remember it’s like nurturing a delicate plant back to health. Stay vigilant with warm baths, fiber-rich foods, and plenty of fluids. If you don’t see improvement in a month, consult your doctor.
Taking these steps seriously ensures you’re tending to your body’s needs, promoting recovery, and preventing future issues.
Prioritize your health this new year, and you’ll find your path to healing smoother than you anticipated.
FAQs
What Is the New Treatment for Fissures?
The new fissure treatment includes dietary adjustments for increased fiber intake, sitz baths to enhance blood flow, topical therapies, and, if needed, Botox injections or laser intervention for effective pain management and healing.
What Happens After Fissure Heals?
You’ve conquered the discomfort; now, post-healing care is critical. Embrace dietary adjustments, increase fiber intake, and maintain hydration importance. Use stool softeners, engage in regular exercise, and don’t skip follow-up evaluations for preventative strategies.
What Should You Not Do With a Fissure?
You should avoid straining, minimize sitting on hard surfaces, skip spicy foods, forgo caffeine, resist scratching, do no heavy lifting, prevent dehydration, avoid constipation, and limit alcohol to protect against aggravating your fissure.
Dr. Rajarshi Mitra is a patient-centered, highly-rated Specialist Laparoscopic Surgeon & Proctologist in Abu Dhabi, offering Advanced Laparoscopic Surgery, Minimally Invasive Proctology & Lasers in Proctology. He is MBBS; MS (Surgery); FIAGES; FICS (USA); Dip. Lap (France); and Dip. Hernia (APHS) with 18 years of extensive experience in Laparoscopic Surgery, Minimally Invasive Proctology and Fellowship training in Colorectal and Bariatric Surgery.